Hoosier state hangs some numbers on prep for COVID-19 patient surge, makes plea for more PPE

After initially declining to provide numerical descriptions of medical resources available to treat COVID-19 patients in the state, Indiana officials have started to quantify some of the ways they’re preparing for the expected surge in patient numbers.
They’re also asking for help in getting more personal protective equipment (PPE) for health workers.
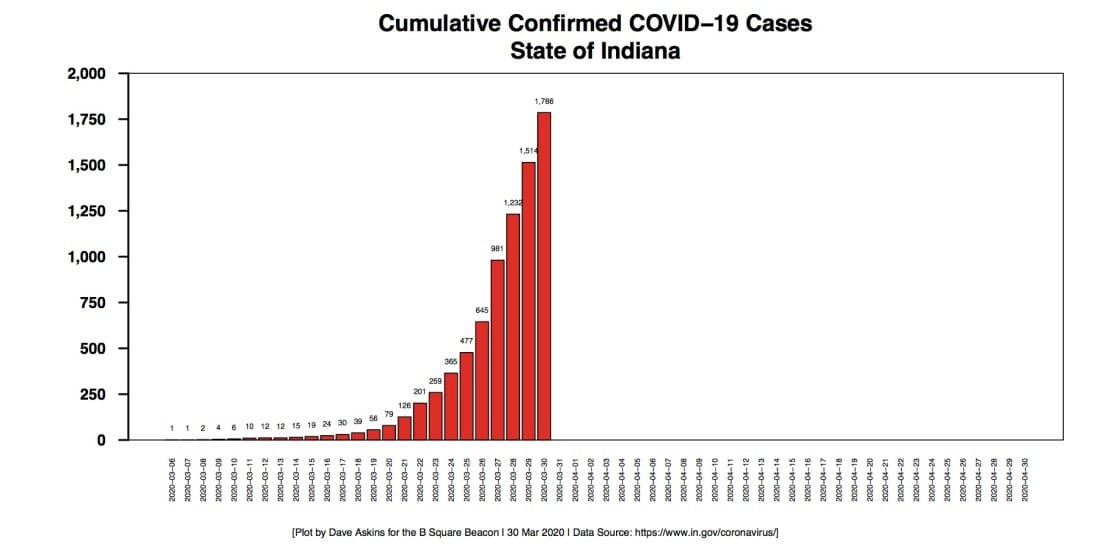
The number of confirmed COVID-19 cases in Indiana has not quite doubled in three days, from 981 on March 27, to 1,786 on March 30. The number of tests that have been done has increased over those days, from 6,936 on March 27, to 11,658 on March 30.
The number of deaths due to COVID-19 in Indiana doubled in four days, from 17 on March 26, to 35 on March 30.
At Indiana governor Eric Holcomb’s daily press conference on Monday, top-level officials gave statewide numbers for two key resources, adding that the numbers could be increased, in some cases at a moment’s notice.
The baseline number of intensive care unit (ICU) beds statewide is 1,432, according to Jennifer Sullivan, a pediatric emergency doctor, who’s secretary of the state’s family and social services administration. At Monday’s press conference, Sullivan said the number of ICU beds has been increased by 35 percent, to 1,940 beds.
About 40 percent of the ICU beds are currently open in the state of Indiana, according to Kristina Box, the state’s health commissioner. Box said that does not match up exactly with the number of open ventilators, because not every patient in an ICU bed needs a ventilator. As of March 1, Sullivan said, there were 1,777 ventilators available statewide.
Several approaches have been taken to adding capacity for ICU beds, which includes converting beds for less acute patients to ICU beds, Sullivan said. The elimination of elective surgery during the COVID-19 pandemic means recovery rooms for some surgical units can be converted to ICU beds, she added.
The general strategies described by Sullivan for adding ICU beds were similar to those described for IU Health’s Bloomington facility last Friday in Bloomington, at a weekly press briefing that included city, county and university officials.
On Friday, Brian Shockney, who’s president of IU Health’s South Central Region confirmed that the hospital has 272 beds and that any rooms where those beds are located can be converted to negative pressure—if they don’t already have a negative pressure environment. That means the space is ventilated in a way that lets air flow into the room but not escape from the room, which helps avoid room-to-room contamination.
“We continue every day to bring more rooms up to negative pressure,” Shockney said on Friday.
Among the specific tactics the Bloomington facility is using to add capacity onsite, Shockney described converting the sleep study area to patient care. Over the years, some areas at the hospital have been turned into surgical check-in areas. Now that only emergency surgery is being done, Shockney said, those check-in areas can be used for patient care.
With the additional beds that the hospital has added onsite, Shockney pegged the total number at over 300.
Doubling the number of ventilators from 1,777 is also a goal for state health officials. Chris Weaver, who’s vice president of clinical and business integration for Eskenazi Health Services, described at Monday’s press briefing one way to add to the number of ventilators: Adapt anesthesia machines in surgical units to function as ventilators. That’s possible, he said, because all elective surgeries have been cancelled during the COVID-19 pandemic emergency.
Weaver said the ventilators statewide are part of a pool, and when a hospital gets close to the edge of their own capacity, they can reach out to the state health department, which will allocate additional ventilators to that hospital.
Weaver stressed that having enough medical equipment is just a part of the response to COVID-19. Having enough people, medical practitioners, is also essential, Weaver said.
Following up on Chris Weaver’s point about having adequate personnel was Lindsay Weaver, who’s the chief medical officer for the Indiana State Department of Health. Lindsay Weaver said 5,300 clinicians statewide have responded to a survey that has been sent out, stepping forward to volunteer their services. The collection of volunteer medical professionals includes retirees, anesthesiologists, trainees, and clinicians who are not currently working because of the current ban on elective surgeries.
Lindsay Weaver also said that the state’s department of health is working with the Indiana University school of medicine to sort out how soon-to-be graduates can be enlisted in the effort to treat COVID-19 patients.
An order signed by Holcomb on Monday allows for retirees, medical students, medical residents, students in some medical fields, and out-of-state medical professionals to get temporary authorization to provide health care services during the COVID-19 emergency.
The personal protective equipment that medical staff need—masks, face shields and gowns—in order to keep themselves from getting infected, continues to be in short supply. That’s in spite of deliveries to Indiana from the National Strategic Stockpile. In two shipments from the stockpile, the state received a total of 126,260 N95 masks, accordion to a slide shown during Lindsay Weaver’s presentation. Indiana’s department of corrections is now manufacturing masks, face shields and gowns, each of those items at a rate of 200 per day.
“Masks are our most needed supply,” Shockney said at last Friday’s press conference in Bloomington. Masks are now being used on patients, he said, given what’s now known about how the virus sheds. Assuming the current usage rate, Shockney said, there’s about a 45-day supply.
A week ago, Bloomington city councilmember Dave Rollo called for an effort to ensure that grocery store workers wear masks, to protect themselves and customers. In the last couple of days, he told The Square Beacon, he has focused on the question of whether health care workers in the Bloomington area have access to adequate numbers of masks, after hearing anecdotal reports that they did not.
On the topic of personal protective equipment, at the governor’s Monday press conference, Lindsay Weaver said, “We are searching for every piece we can find.” If you can assist, she said, please send an email message to: COVIDResponse@iedc.IN.gov
Based on the models developed by researchers in Indiana and by ISDH staff, Sullivan said during Monday’s press conference that she believes the patient peak surge will come sometime in mid-April to mid-May. That’s a slight shift from the thinking last week, when the timeframe for the expected peak was mid-April to late-April.
Also showing a slight shift was a model released on Friday by the Institute for Health Metrics and Evaluation (IHME), which initially forecasted the peak patient surge for Indiana to come on April 14. By Monday, the IHME model had pushed the peak to April 17. The institute is a health research center at the University of Washington.
Compared to the Friday forecast for Indiana by the IHME model, on Monday it was predicting far fewer resources needed for the peak as well as far fewer total deaths from the disease.
On Friday, the model was predicting that 1,582 ICU beds would be needed for the peak. The forecasted peak number of ICU beds is now down to 503. In the IHME model, the forecasted number of ventilators that will be needed statewide dropped from 854 to 402. The forecasted number of total deaths dropped from 2,440 to 940.
Asked by a reporter about the IHME model at Monday’s press conference, Sullivan said there’s a wide range between the best- and worst-case scenarios. Like any model, she said, the IHME model forecast will change, when the data that is put into it changes.
What might have changed? Over the weekend, Sullivan said, the number of additional deaths in Indiana was low. After jumping by 14, from 17 to 31, between March 26 and March 28, the number of deaths over the following two days rose by 4.
Sullivan said that it was not cause for celebration, and the state’s health officials will continue to plan for a significant surge in patient numbers.


Comments ()