Column: On the normalcy of local COVID-19 response



Early Friday afternoon, Monroe County’s health administrator, Penny Caudill,
sent out a press release announcing the county’s first confirmed case of COVID-19, the pandemic virus that’s spreading across the world.
It was a student seen a week earlier by Indiana University Health Center, whose positive test was reported to the center just that morning.
The student, who lives off-campus, self-isolated for the week while the test was being processed. The student health center sent the test to LabCorp, a private lab in Burlington, North Carolina, according to the student health center’s medical director, Beth Rupp.
The COVID-19 infection that was reported on Friday appears to be a case contracted in Monroe County. Rupp told a group of reporters on a Zoom video conference call on Friday that the student had not travelled recently and had no known exposure.
Rupp confirmed that LabCorp reported the positive result to the health center on Friday morning. Rupp said her first step was to contact the patient. After that, the student health center notified Caudill, as Monroe County’s health administrator.
Caudill was a part of Friday afternoon’s press conference call, which was organized by Indiana University’s director of media relations, Chuck Carney.
One of my takeaways from the conference call was mostly a confirmation of the grim conclusion that several reliable, data-driven sources support: Monroe County, Indiana, will not escape the impact of COVID-19. And the scale of that impact will be significant.
As Caudill put it on Friday: “We have been expecting it—I think every community in Indiana and the nation, if they haven’t had a confirmed case, they have been expecting it and planning for it.” Caudill said people should expect the number of Monroe County cases to increase.
The other key point I took from the call was a little more optimistic: COVID-19 has a place in the normal routine that public health departments use for dealing with communicable diseases generally, even if the scale will likely be unprecedented.
Caudill and Rupp sketched a still grim, if improving picture of COVID-19 testing availability. When the outbreak first hit, samples could be sent only to Indiana’s State Department of Health (ISDH), because that was the only place with testing capability that was available to local heath providers.
Initial tests sent to ISDH had to meet strict criteria, including that a patient be “high risk,” based on the Center for Disease Control definition: over 65 years older; or with underlying health conditions like heart disease, lung disease, diabetes; or with a weakened immune system.
Around March 12 or so, the IU student health center’s “reference lab”—the facility to which it refers diagnostic tests—got the ability to do COVID-19 tests. That meant the health center, and other local health providers who have access to COVID-19 reference labs, could relax their criteria for testing. But only somewhat. Rupp said the limiting factor now is the amount of the media the student health center has on hand for storing the specimens to send to the lab.
So the basic advice, as of Friday, remains: If you think you have COVID-19 symptoms— fever, tiredness, and dry cough—stay home, call your health provider, but don’t venture out on an expedition trying to find a way to get tested.
On Friday, Rupp said the student health center had sent a total of one test to the state health department and 11 others to LabCorp. Of the 12 tests, one had come back positive for COVID-19, three had come back negative, and eight were still pending, Rupp said.
As sobering as the conference call was, I found some modest reassurance in the information Rupp and Caudill provided.
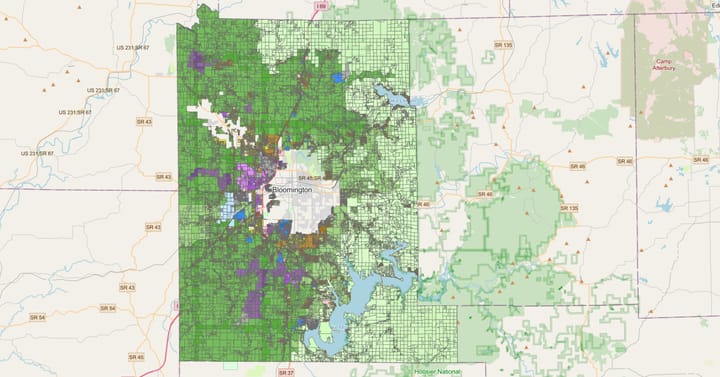
Caudill confirmed what the label on the state’s information dashboard says: COVID-19 cases are counted by the county of residence for the patient. So cases are not logged by the location of the treatment facility. (There’s at least one case where a COVID-19 patient didn’t get logged in the correct county. The news release from ISDH on Sunday, March 22, said a confirmed case initially logged for Hancock County was changed to Marion County.)
Reporting of cases to the public, based on the county of residence of the patient, is not an approach that was adopted especially for COVID-19. As Caudill described it: “Virtually all communicable diseases are reported by somebody’s county of residence. So that is typically the way they are reported.”
Another way that COVID-19 fits into routine public health reporting involves how news of positive cases is relayed to public health officials. Rupp described how LabCorp reported the positive result to the health center on Friday morning. After contacting the patient, Rupp’s office notified Caudill, Monroe County’s health administrator.
Notifying the county health department wasn’t some extra precaution that Rupp was following that was put in place just for COVID-19. It’s required reporting for communicable diseases generally, under the Indiana Administrative Code. It is Title 410 of the state code covers reporting requirements for dangerous communicable diseases and disease intervention measures.
Caudill pointed out on Friday that the reporting to her department of the confirmed IU student case was not enough to make it show up on the ISDH dashboard as a Monroe County case. Just the results that ISDH gets from private labs and its own testing are included in the dashboard.
That’s why there was a lag between Friday’s positive test and Sunday’s first appearance of the case on the ISDH map. LabCorp notified IU’s student health center Friday morning. about the positive test. But Caudill indicated that it was LabCorp’s report to IDHS that would make the dashboard tally increment upward for Monroe County, not a report to the state from her office or the IU student health center.
A more substantive way that COVID-19 fits into the normal routine of handling communicable diseases applies to the “contact tracing” that Caudill’s public health nurses are now conducting on the COVID-19-positive student. Those nurses are also IU Health employees—there’s a partnership between the county health department and IU Health for public health nursing services, according to Caudill.
Contact tracing means figuring out who the patient came in contact with, and then communicating directly with those contacts, so that they can be advised about how they should protect themselves and others. About the idea that a contact might not be locatable, Caudill told The Square Beacon, “Since this [COVID-19] infection seems to require close contact for prolonged time there shouldn’t be expectation of not being able to locate someone.”
The task of contact tracing is not something new to county public health nurses, that they had to learn in order to deal with the COVID-19 pandemic.
As Caudill put it: “The health department does follow-up contact tracing in communicable diseases every day. This is something that our nurses and other staff are trained in and they do very, very well.” She added, “That’s what we do with gonorrhea, it’s what we do with HIV, syphilis, tuberculosis and other communicable diseases.”
Obviously, COVID-19 is not like any other communicable disease. And I don’t mean to imply that we should consider it as anything but a dangerous disease that we should take every precaution to prevent. It’s a disease for which we should start to contemplate scenarios where we or someone we know becomes infected.
It’s part of a journalist’s job is to be skeptical of anything a public official says. But the county public health department’s response to COVID-19 is in its wheelhouse. That helps give me some added confidence that I can, as a regular citizen, at least trust the advice that the county health department is dispensing.
If Penny Caudill says to wash my hands, again, I’m going to do it.


Comments ()